I just ran across this meta-analysis of antibody test performance on medrxiv:
Antibody tests in detecting SARS-CoV-2 infection: a meta-analysis
In total, we identified 38 eligible studies that include data from 7,848 individuals. The analyses showed that tests using the S antigen are more sensitive than N antigen-based tests. IgG tests perform better compared to IgM ones, andshow better sensitivity when the samples were taken longer after the onset of symptoms. Moreover, irrespective of the method, a combined IgG/IgM test seems to be a better choice in terms of sensitivity than measuring either antibody type alone. All methods yielded high specificity with some of them (ELISA and LFIA) reaching levels around 99%. ELISA-and CLIA-based methods performed better in terms of sensitivity (90-94%) followed by LFIA and FIA with sensitivities ranging from 80% to 86%.
The sensitivity results are interesting, but I’m more interested in timing:
Sample quality, low antibody concentrations and especially timing of the test -too soon after a person is infected when antibodies have not been developed yet or toolate when IgM antibodies have decreased or disappeared -could potentially explain the low ability of the antibody tests to identify people with COVID-19. According to kinetic measurements of some of the included studies 22, 49, 54 IgM peaks between days 5 and 12 and then drops slowly. IgGs reach peak concentrations after day 20 or so as IgM antibodies disappear. This meta-analysis showed, through meta-regression, that IgG tests did have better sensitivity when the samples were taken longer after the onset of symptoms. This is further corroborated by the lower specificity of IgM antibodies compared to IgG 15. Only few of the included studies provided data stratified by the time of onset of symptoms, so a separate stratified analysis was not feasible, but this should be a goal for future studies.
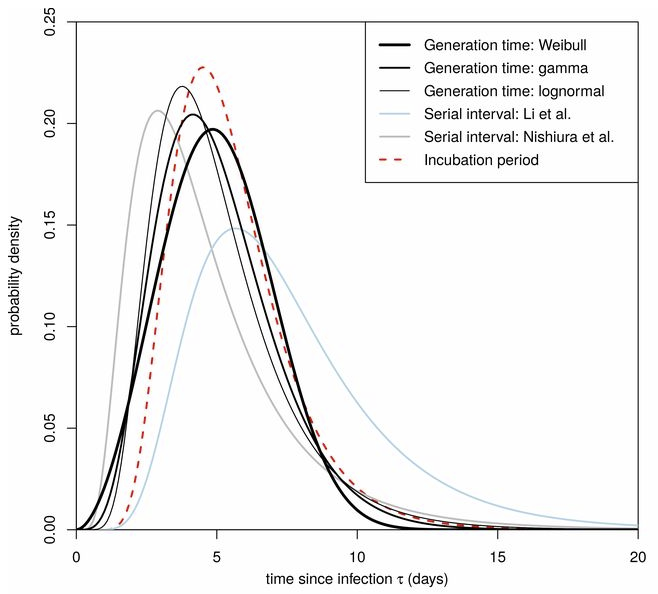
This is an important knowledge gap. Timing really matters, because tests that aren’t sensitive to early asymptomatic transmission have limited utility for preventing spread. Consider the distribution of serial infection times (Ferretti et al., Science):
Testing by itself doesn’t do anything to reduce the spread of infection. It’s an enabler: transmission goes down only if coronavirus-positive individuals identified through testing change their behavior. That implies a chain of delays:
- Conduct the test and get the results
- Inform the positive person
- Get them into a situation where they won’t infect their coworkers, family, etc.
- Trace their contacts, test them, and repeat
A test that only achieves peak sensitivity at >5 days may not leave much time for these delays to play out, limiting the effectiveness of contact tracing and isolation. A test that peaks at day 20 would be pretty useless (though interesting for surveillance and other purposes).
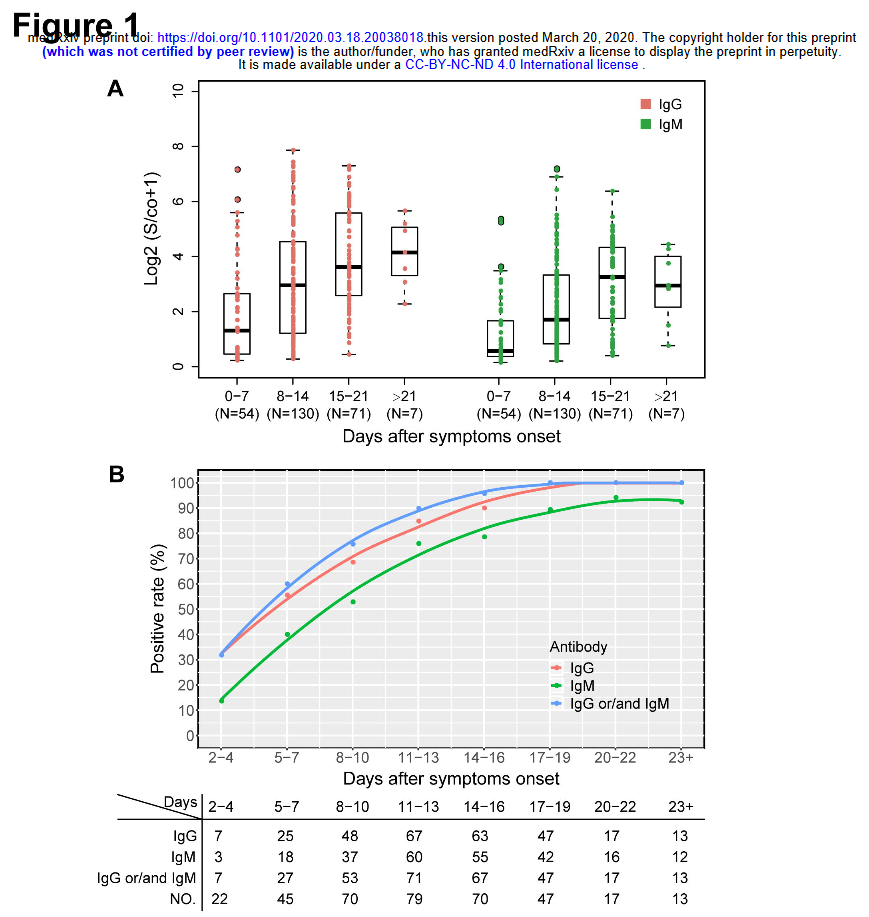
Seroconversion rates of 30% at onset of symptoms seem problematic, given the significant pre-symptomatic transmission implied by the Ferretti, Liu & Nishiura results on serial infection times. I hope the US testing strategy relies on lots of fast tests, not just lots of tests.
See also:
Antibody surveys suggesting vast undercount of coronavirus infections may be unreliable in Science
h/t Yioryos Stamboulis