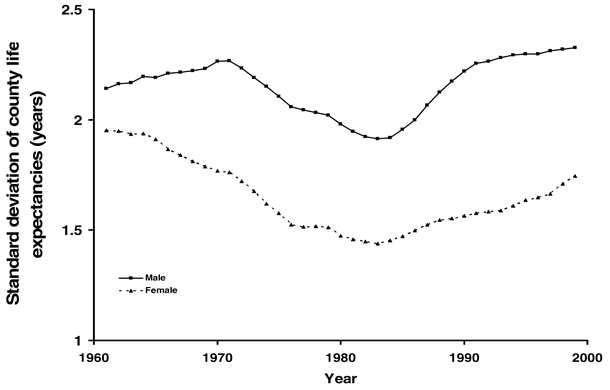
Today ScienceDaily brought the troubling news that, “There was a steady increase in mortality inequality across the US counties between 1983 and 1999, resulting from stagnation or increase in mortality among the worst-off segment of the population.” The full article is PLoS Medicine Vol. 5, No. 4, e66 doi:10.1371/journal.pmed.0050066. ScienceDaily quotes the authors,
Ezzati said, “The finding that 4% of the male population and 19% of the female population experienced either decline or stagnation in mortality is a major public health concern.” Christopher Murray, Director of the Institute for Health Metrics and Evaluation at the University of Washington and co-author of the study, added that “life expectancy decline is something that has traditionally been considered a sign that the health and social systems have failed, as has been the case in parts of Africa and Eastern Europe. The fact that is happening to a large number of Americans should be a sign that the U.S. health system needs serious rethinking.”
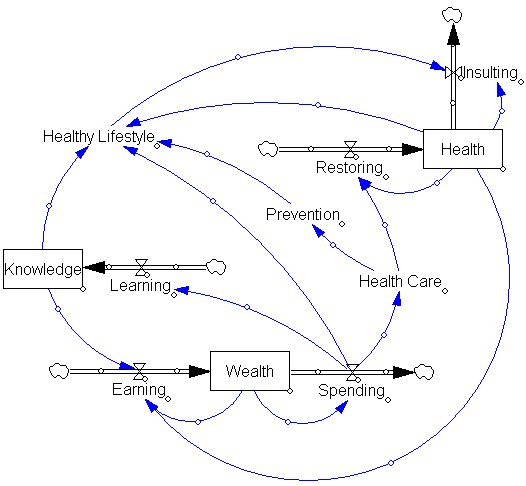
I question whether it’s just the health system that requires rethinking. Health is part of a complex system of income and wealth, education, and lifestyle choices:
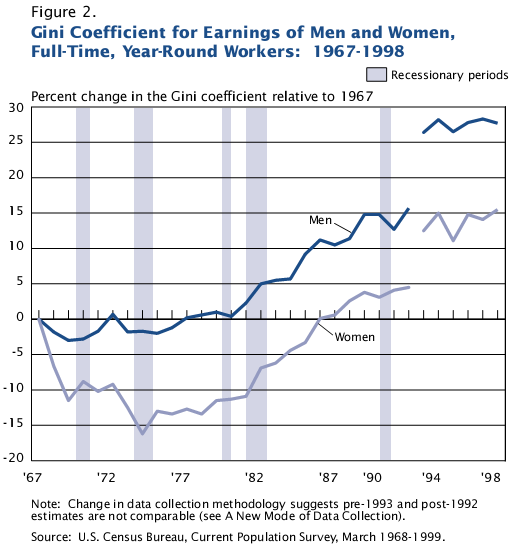
Health care, particularly restorative care, may simply be on the losing end of other feedbacks that are driving rising income inequality and unhealthy lifestyles. It could also play an intimate role in mitigating or amplifying those processes. It is at least provocative to compare the authors’ trajectory of health inequality with the Census’ trajectory of income inequality:
It would be overreaching to say that health trends look like a delayed version of the income signal, but there are enough similarities to prompt reflection on whether health care, particularly therapy, is the only point of leverage in the system.
For a useful overview of modeling the complexity of health care, see this article by Jack Homer & Gary Hirsch.