I’ve been looking at early model-based projections for the coronavirus outbreak (SARS-CoV-2, COVID-19). The following post collects some things I’ve found informative. I’m eager to hear of new links in the comments.
This article has a nice summary, and some
Disease modelers gaze into their computers to see the future of Covid-19, and it isn’t good
The original SIR epidemic model, by Kermack and McKendrick. Very interesting to see how they thought about it in the pre-computer era, and how durable their analysis has been:
A data dashboard at Johns Hopkins:
A Lancet article that may give some hope for lower mortality:
The CDC’s flu forecasting activity:
Some literature, mostly “gray” preprints from MedRxiv, all open access:
- BeyondR0: the importance of contact tracing when predicting epidemics
- The Novel Coronavirus, 2019-nCoV, is Highly Contagious and More Infectious Than Initially Estimated
- A simple model for behaviour change in epidemics
- Notes on R0
- SARS: Lessons from Toronto
- Risk Assessment of Novel Coronavirus COVID-19Outbreaks Outside China
A podcast with some background on transmission from Richard Larson, MIT (intestine alert – not for the squeamish!):
- Resoundingly Human: A look inside the rapid spread of the coronavirus, what are we missing?
This blog post by Josh at Cassandra Capital collects quite a bit more interesting literature, and fits a simple SIR model to the data. I can’t vouch for the analysis because I haven’t looked into it in detail, but the links are definitely useful. One thing I note is that his fatality rate (12%) is much higher than in other sources I’ve seen (.5-3%) so hopefully things are less dire than shown here.
I had high hopes that social media might provide early links to breaking literature, but unfortunately the signal is swamped by rumors and conspiracy theories. The problem is made more difficult by naming – coronavirus, COVID19, SARS-CoV-2, etc. If you don’t include “mathematical model” or similar terms in your search, it’s really hopeless.
If your interested in exploring this yourself, the samples in the standard Ventity distribution include a family of infection models. I plan to update some of these and report back.
This one is a bit older – could not find an update: https://www.medrxiv.org/content/10.1101/2020.01.23.20018549v2
From what I have learnt from doctors is that the fatality numbers luckily seem to come out at the lower end and the expected scenario is similar to a severe flu. They also point out that there are dynamics at play in identification of cases: In the beginning no one knows what to look for or only few are looking. Cases identified are late stage with high mortality. Then the pendulum swings back, people getting overanxious, governments overreact to show leadership (that is what the doctors seem to be most annoyed of btw). It takes a while for threat and response to become aligned.
Also I think response levels by country vary significantly. On one end of the spectrum you have autocrat states with almost full media control and dysfunctional government, on the other end states with full public health system coverage which have begun to ramp up the emergency response infrastructure weeks ago, execute counter measures and communication as preplanned according to the threat level and then there are states in between. Infection rates and mortality will vary.
A good summary from the NYT:
https://www.nytimes.com/interactive/2020/world/asia/china-coronavirus-contain.html
A nice article on flu forecasting model considerations:
https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1005964
More data dashboards:
https://www.worldometers.info/coronavirus/covid-19-testing/
https://www.mongodb.com/blog/post/tracking-coronavirus-news-with-mongodb-charts
Unfortunately the github data repositories for these (and the Johns Hopkins source at top) seem to be lagging a bit.
An H1N1 model projection retrospective:
https://academic.oup.com/eurpub/article/22/1/7/489927
Seasonality – will there be a little peak now, and a bigger one next fall?
https://www.medrxiv.org/content/10.1101/2020.02.13.20022806v2
The serial interval between infections is shorter than the incubation period, indicating that the asymptomatic exposed may be infectious:
https://www.medrxiv.org/content/10.1101/2020.02.03.20019497v2
The effect of human mobility and control measures on the COVID-19 epidemic in China
https://www.medrxiv.org/content/10.1101/2020.03.02.20026708v1
How does the outbreak of 2019-nCoV spread in mainland China? A retrospective analysis of the dynamic transmission routes
https://www.medrxiv.org/content/10.1101/2020.03.01.20029645v1
JAMA Network COVID-19 resource page:
https://jamanetwork.com/journals/jama/pages/coronavirus-alert
Evolving Epidemiology and Impact of Non-pharmaceutical Interventions on the Outbreak of Coronavirus Disease 2019 in Wuhan, China
https://www.medrxiv.org/content/10.1101/2020.03.03.20030593v1
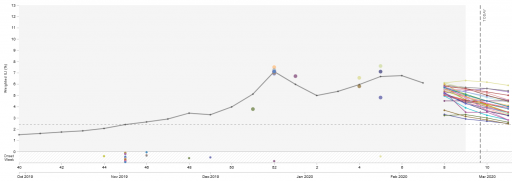
“The effective reproductive number dropped from 3.86 (95% credible interval 3.74 to 3.97) before interventions to 0.32 (0.28 to 0.37) post interventions. “
Effects of weather-related social distancing on city-scale transmission of respiratory viruses
https://www.medrxiv.org/content/10.1101/2020.03.02.20027599v1
Time-varying estimates of R0, from a deep dive into the timing of individual case reports: https://cmmid.github.io/topics/covid19/current-patterns-transmission/global-time-varying-transmission.html
https://cmmid.github.io/topics/covid19/current-patterns-transmission/overdispersion-from-outbreaksize.html
“…the majority of secondary transmission is caused by a very small fraction of individuals (80% of transmissions caused by ~10% of the total cases).”
Pre-symptomatic transmission is 25-30% of cases:
https://cmmid.github.io/topics/covid19/control-measures/pre-symptomatic-transmission.html
Transmission interval estimates suggestpre-symptomatic spread of COVID-19
https://www.medrxiv.org/content/10.1101/2020.03.03.20029983v1.full.pdf
Imperial College report on UK with detailed assumptions and different policy outcomes:
https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf
You’re faster than me. Was just looking at that. Thanks!
A website near real time which tells you the COVID-19 numbers. The site was created by a 17 year kid.
Thanks! Sorry for delay – posts with links get moderated first time.
https://ncov2019.live/
Good discussion in the Lancet:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30567-5/fulltext
How will country-based mitigation measures influence the course of the COVID-19 epidemic?
Governments will not be able to minimise both deaths from coronavirus disease 2019 (COVID-19) and the economic impact of viral spread. Keeping mortality as low as possible will be the highest priority for individuals; hence governments must put in place measures to ameliorate the inevitable economic downturn. In our view, COVID-19 has developed into a pandemic, with small chains of transmission in many countries and large chains resulting in extensive spread in a few countries, such as Italy, Iran, South Korea, and Japan.1
Most countries are likely to have spread of COVID-19, at least in the early stages, before any mitigation measures have an impact.
What has happened in China shows that quarantine, social distancing, and isolation of infected populations can contain the epidemic.1
This impact of the COVID-19 response in China is encouraging for the many countries where COVID-19 is beginning to spread. However, it is unclear whether other countries can implement the stringent measures China eventually adopted. Singapore and Hong Kong, both of which had severe acute respiratory syndrome (SARS) epidemics in 2002–03, provide hope and many lessons to other countries. In both places, COVID-19 has been managed well to date, despite early cases, by early government action and through social distancing measures taken by individuals.
Summarizes a lot of the lit on incubation, asymptomatic transmission, etc.
Very interesting study of CFR. The results seem plausible for the UK, but I’m less convinced for places like Indonesia.
Using a delay-adjusted case fatality ratio to estimate under-reporting
https://cmmid.github.io/topics/covid19/severity/global_cfr_estimates.html
In real-time, dividing deaths-to-date by cases-to-date leads to a biased estimate of the case fatality ratio (CFR), because this calculation does not account for delays from confirmation of a case to death, and under-reporting of cases.
Using the distribution of the delay from hospitalisation-to-death for cases that are fatal, we can estimate how many cases so far are expected to have known outcomes (i.e. death or recovery), and hence adjust the naive estimates of CFR to account for these delays.
The adjusted CFR does not account for under-reporting. However, the best available estimates of CFR (adjusting or controlling for under-reporting) are in the 1% – 1.5% range. We assume a baseline CFR, taken from a large study in China, of 1.38% (95% crI: 1.23–1.53%)[6]. If a country has an adjusted CFR that is higher (e.g. 20%), it suggests that only a fraction of cases have been reported (in this case, 1.3820=6.9%
cases reported approximately).
I assume it makes a significant difference for the policy response if a country has almost 100% transparency about total cases (I saw some overview from Australia where they show that they can trace back almost all cases) e.g. to decide when to move to more broad-brush responses.
Here is a model of the Boston area assessing the impact of social distancing strategies: https://covid-19-sds.github.io/