My last post probably sounds like I disagree with Jack Homer’s recommendation to tolerate some exogenous drivers and consideration of policy feasibility. Actually I don’t. In fact, we at Ventana probably do more data-intensive SD than anyone. I build hybrid models all the time.
When philosophizing about the best way to change the world, it’s easy to lose sight of some practical considerations that influence choices:
- Cost. It’s expensive to develop an elegant, endogenous theory for things like interest rates that you might normally think of as exogenous to a firm. On the other hand, it’s also expensive to collect and use data – often 1/3 of project cost in our experience.
- Clarity. Exogenous variables complicate the analysis of a model, because you have driven behavior on top of the model’s endogenous dynamics. I think this makes it harder to understand the basic behavior, because you lose the insight you might gain from starting a model in equilibrium and perturbing it with policies.
- Calibration. On the other hand, using exogenous drivers increases your ability to gain insight from comparison of model behavior to data. This is not a definitive test, but you can definitely use it to estimate uncertain parameters and weed out certain dumb ideas.
- Client. You have to meet people where they are. If, historically, they think R^2 is the definitive measure of success, you’d better deliver. You can explain why that’s a bad metric and present a more endogenous view of the situation later, after you’ve established trust.
I think there’s no clear answer – the extent to which endogenous or exogenous elements are preferred has to be a situation-specific decision. In my own work, I often use a two-pronged approach, and two ways to structure that have emerged:
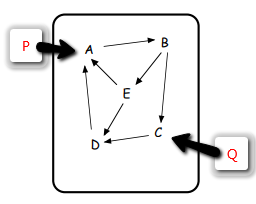
- Build a single, large, calibrated model with some exogenous drivers. Build endogenous submodels or metamodels for equilibrium experiments and to explain key features of the big model.
- Build a single, elegant endogenous model, with few drivers. Use smaller exogenous models, or statistical and machine learning tools, to understand local features of the data, incorporating those insights into the endogenous model without using the data directly.